For years, osteoporosis medication has been the standard for many women to maintain good bone health. You will want to discuss new findings with your doctor. A troubling link was discovered between long-term use of common osteoporosis medications and an increased risk of breaking thigh bones. Although these medications, commonly used in millions, do prevent fractures and build bone density, over time, the treatments can have the opposite effect on some patients: the femur may weaken.
Osteoporosis Drugs and Thigh Fractures: The Disturbing Connection
The Unexpected Side Effect
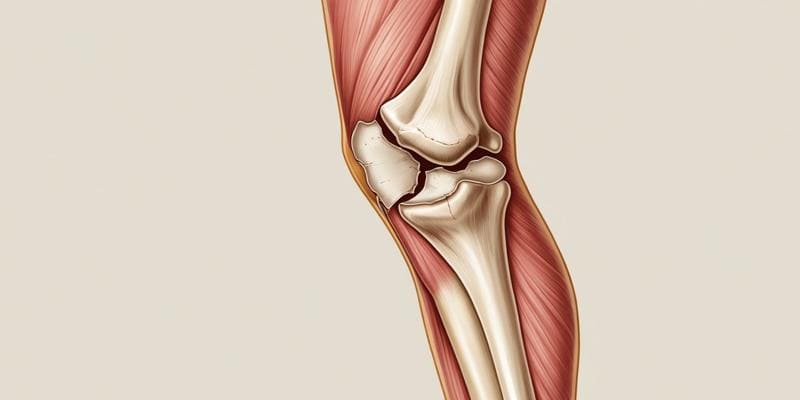
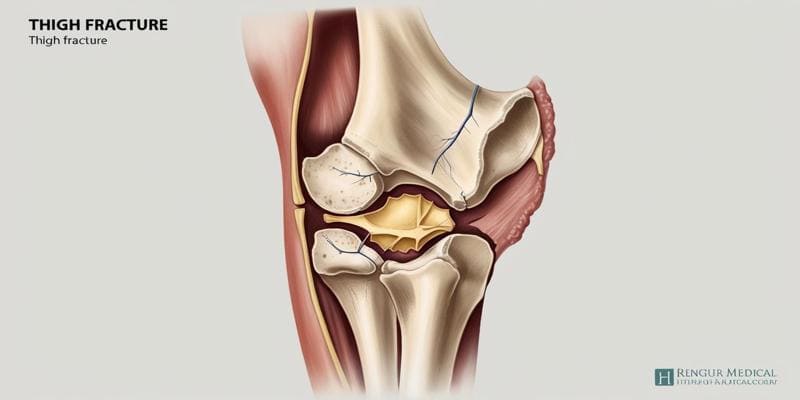
Osteoporosis treatment has rested on the mainstay of bisphosphonates for many years, helping to fortify bones in millions and reduce the risk of fractures. Recent studies, however, have unearthed a paradoxical and disturbing side effect: an increased risk of atypical femur fractures. These rare but serious breaks occur in the thigh bone, often with little or no trauma, and can be devastating for patients.
Understanding the Mechanism
This risk may be related to the very action that renders bisphosphonates effective in the treatment of osteoporosis. Usually, the bone remodelling process continuously repairs bone tissue, but these drugs slow it down. While this helps maintain bone density, thereby preventing fractures, it tends to allow microdamage in the bone to accumulate over years. This may favour the fracturing of a weakened femur.
Weighing the Risks and Benefits
However, for most patients, the benefits they see from bisphosphonate therapy are still in excess compared to the risks. Indeed, overall fracture prevention has resulted from these drugs, especially in those that are considered at high risk. Still, this discovery has now led to reassessments on the use of these agents long-term; most authors now advocate a "drug holiday" after 3 to 5 continuous years of drug administration to provide some reprieve and renormalisation of the bone remodelling processes by the body.
Moving Forward: Personalized Treatment Approaches
Looking Ahead: Individualized Treatment Strategies This new knowledge emphasises individualised treatment strategies for osteoporosis. The duration of the treatment with bisphosphonates is based on age, any previous history of fracture, and bone density measurement. The trade-off between prevention of osteoporosis and possible long-term risk requires close follow-up, and good communication between the patient and clinician is a prerequisite.
Understanding Atypical Femoral Fractures Linked to Long-Term Osteoporosis Medication Use
The Unexpected Side Effect
Atypical femoral fracture is a rare but serious adverse effect of long-term use of osteoporosis medications, especially bisphosphonates. The fractures in the thigh bone, better known as the femur, are defined by their unusual location and pattern. Other than that, they do not usually occur from falling, as is the case with usual osteoporotic fractures; atypical fractures may happen with little or no trauma and even while performing everyday activities like walking or standing.
Identifying the Risk Factors
Several risk factors have been identified which further predispose long-term bisphosphonate users to atypical femoral fractures:
- Duration: The risk increases after 3-5 years of continuous bisphosphonate therapy.
- Genetic predisposition: Because of genetic background, some people may be more susceptible to this condition.
- Combination drugs: There are certain drugs, like glu and corticoids, that can increase the risk
- Bone geometry: The shape of the femur or bone density may be other contributing factors
Recognising the Warning Signs
Patients who are on bisphosphonates for some years should know possible warning signs that may include:
- Dull, aching pain in the groin or thigh
- Difficulty in walking or standing for some time
- Suddenly, sharp pain in the thigh while doing daily activities
Early identification of such symptoms leads to interventions to avoid a fracture.
Balancing Benefits and Risks
While the risk of atypical femoral fractures is a concern, it needs to be emphasised that for many patients, the benefits of bisphosphonate therapy in preventing osteoporotic fractures still outweigh the risks. However, this does stress the need for individualised treatment plans and regular reassessment regarding medication efficacy and safety. Providers should, therefore, be considering drug holidays or alternative therapies for those patients on long-term bisphosphonate treatment, especially for those at higher risk of developing an atypical femoral fracture.
Risks and Benefits: Weighing the Pros and Cons of Long-Term Osteoporosis Medication
Understanding the Potential Benefits
While there is a risk of atypical femoral fractures, the benefit of bisphosphonate therapy in preventing an osteoporotic fracture outweighs the risks in many patients. Again, that puts into perspective the principles of individualising treatments and regular reassessment regarding medicines' efficacy and safety. For patients who have been on bisphosphonates for many years, healthcare providers should consider either a drug holiday or other treatments for those patients who have a higher risk of atypical femur fractures.
Considering the Risks
But over the years, concerns about their long-term safety have been raised. Of these, a potential link between long-term bisphosphonate use and atypical femur fact is probably the most disturbing. These uncommon but sometimes catastrophic fractures can occur with minimal trauma and prove resistant to healing. Other possible long-term side effects seen in some patients include devastating jaw problems, such as osteonecrosis.
Balancing Act: Personalized Treatment Approaches
These competing interests raise several red flags that call for clinicians to balance the treatment of osteoporosis further. This includes the following:
- Routine reestimation of fracture risk
- Drug holidays after 3-5 years of treatment
- Medication regimens tailored to individual patient factors
The benefits of factors such as fracture prevention have to be weighed against the possible risks of long-term therapy. Each case is different, and patients should discuss their specific case with their healthcare professional based on such factors as age, history of fractures, and current condition.
Alternatives to Traditional Osteoporosis Drugs for Bone Health
Natural Approaches to Strengthen Bones
Where prescription drugs have been the traditional avenue to manage osteoporosis for so many years, new worries over their long-term consequences are encouraging people to look at natural options for protecting the bones. Fortunately, several natural interventions are available to strengthen bones and prevent fractures. Exercise and lifestyle modification
Exercise and Lifestyle Modifications
Regular weight-bearing and resistance exercises are essential to maintaining good bone health. The best activities for bones include walking, jogging, dancing, and weight training because these activities stimulate bone growth and may help prevent bone loss. Aim for at least 30 minutes of moderate exercise most days of the week.
Conclusion
Any decision regarding pharmacologic intervention for osteoporosis must balance the risks versus the benefits. Although these medications are quite effective for increasing bone density for many, their serious yet rare side effects cannot be completely ignored as offset against long-term issues of bone health. Discuss your risk factors and options with your doctor.












